一月1
CareOregon responsibilities greatly expand under CCO 2.0
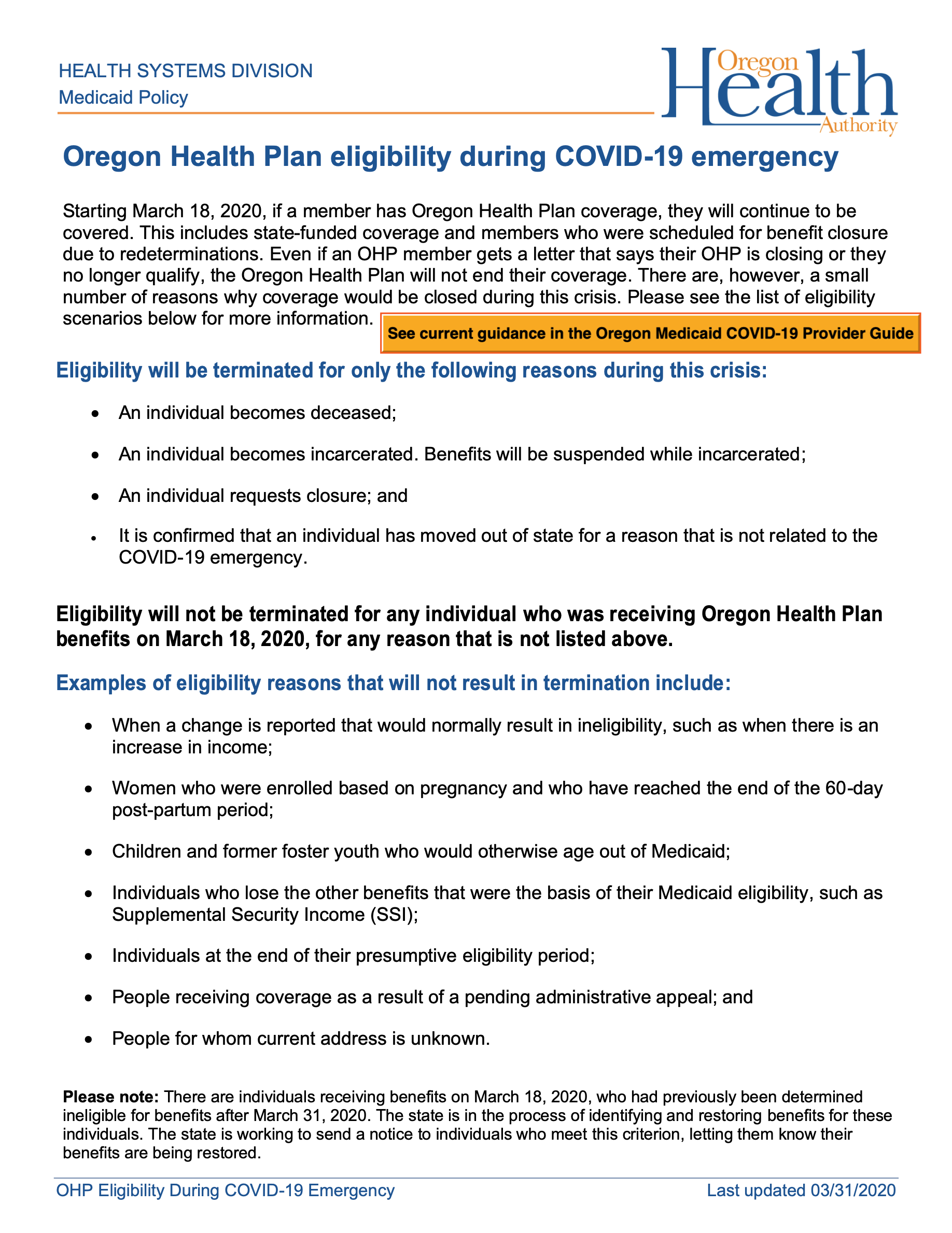
The new decade brought a new day for coordinated care organizations (CCOs). “CCO 2.0” – the next iteration of Oregon’s health care reform – launched January 1, following a year of preparations. It meant revised contracts between the Oregon Health Authority (OHA) and the 16 CCOs across the state.
The CCO 2.0 contracts spelled out one- or five-year agreements, and we were pleased that OHA awarded five years to CareOregon’s two CCOs (Columbia Pacific CCO and Jackson Care Connect) and Health Share of Oregon, our partner CCO in the Portland tri-county area.
Under these contracts, we accepted expanded responsibilities. They represented the progression of our decision, back in 1993-94, to help create an innovative managed care plan dedicated to Oregon Health Plan (OHP) clients. As the state’s health reform evolved to coordinated care organizations in 2012, the intent was to deliver comprehensive care. CCO 2.0 was another big step in offering a holistic approach that combined physical, dental and mental health care.
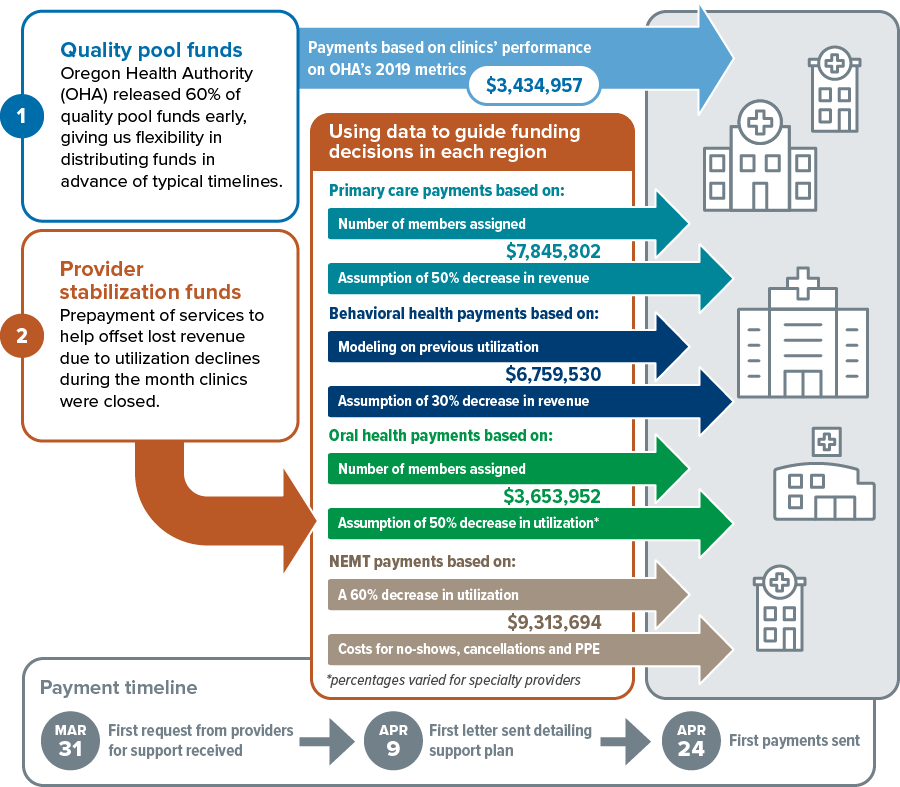
For the CareOregon family, CCO 2.0 brought changes in behavioral health, non-emergent medical transportation (NEMT) and oral health. At the same time, Jackson Care Connect saw a sharp, overnight rise in membership due to a decision by a major provider network.
行为健康
We began serving all Health Share members’ needs for mental health care and substance use treatment, which better allowed for integrated care delivery and administrative efficiencies, says Jill Archer, Vice President, Behavioral Health.
At the start of 2020, before the pandemic changed all expectations, the behavioral health team expected to be refining our contracts and processes for interacting with the nearly 200 behavioral health providers we’d engaged to serve more than 300,000 Health Share members.
NEMT
Providing free transportation to covered health care visits is a complicated undertaking.
In CCO 2.0, CareOregon took responsibility for this important benefit. In January we continued the immense amount of preparation and soft launches of different aspects of handling NEMT for all Health Share members, with eyes on a full handover from Health Share in March 2020.
Working with transportation experts that make up Ride to Care, a transportation program serving Clackamas, Multnomah and Washington counties, we assembled an initial network of 65 subcontracted NEMT transportation providers, says Jen Martinek, Strategic Business Partnership Manager. With the help of new NEMT-scheduling software and live GPS data tracking, we began planning and testing a sustainable process capable of offering nearly a million transit passes, trip reimbursements and vehicle-provided rides to eligible members in the year ahead.
Oral health
For the first time ever, CareOregon Dental moved beyond the Portland tri-county area with its services. With CCO 2.0 dawned a partnership with Tillamook County Community Health Centers. In January, CareOregon Dental became a second dental plan serving Columbia Pacific CCO members, along with Willamette Dental. We onboarded more than 4,750 child and adult dental members who live in Tillamook County.
We entered the region with a great deal of ideas and plans, says Alyssa Franzen, DMD, Vice President, Dental, and excitement about the opportunity to collaborate with physical health practitioners and patients.
In the Portland area, Dental was part of a significant shift of CareOregon members to health homes that are able to provide both primary care and dental services. Aligning physical and oral health services, particularly at federally qualified health centers (FQHCs), offers members the chance for more cohesive, streamlined care.
Jackson Care Connect membership
With the flip of the calendar to January 1, our CCO in Jackson County took on more than 10,500 new members. This large jump – from 33,260 members to 43,849, an increase of nearly one-third – was the outgrowth of an earlier decision by the board of PrimeCare.
PrimeCare, a provider network representing more than 500 doctors in the Medford area, had decided it could best serve OHP members by contracting mainly with a single CCO. We’re grateful the network chose Jackson Care Connect. In welcoming and serving this flood of new members, we focused on continuity of care for them, and close communication with our provider network and the OHA. See details in Jackson Care Connects’s Report to the Community.
Other 2020 commitments
Across the CareOregon family, we greeted the ’20s ready to expand our language interpretation and translation services. We also carried forward our commitment to focus on housing and trauma-informed care, and provide equitable, accessible and culturally competent health care. By investing in individuals and communities, we are determined to keep progressing in reducing health disparities as we make health care work for everyone.




















_page_1.jpg?sfvrsn=39baf920_4)
_page_2.jpg?sfvrsn=a9a37949_4)