新闻和故事
All stories
Stories that highlight the people and programs making healthcare more accessible across Oregon.
Company highlights
The innovative programming and achievements that reflect our commitment to quality care.
CareOregon culture
A look inside the people and values that make CareOregon a compassionate workplace.
Community impact
Partnerships and programs that strengthen health and wellbeing across Oregon communities.
Health and wellness
Tips and insights to support physical and emotional wellbeing for our members.
Strengthening Oregon’s health care workforce: Preparing for tomorrow, today

The power of Medicaid at work
Across United States, health care faces a “perfect storm” of challenges — workforce shortages, rising care costs and widening disparities in health outcomes. In Oregon, these problems are amplified by a mental health crisis and limited access to care.
While barriers exist statewide, they look different depending on where you live. Rural communities often face higher poverty rates and have fewer specialists, while urban areas grapple with provider burnout.
CareOregon is committed to strengthening the health care workforce across Oregon, investing in programs and services that support both urban and rural communities. That commitment starts with investing in people and building a workforce pipeline that prepares future health leaders, strengthens rural health systems and supports community based care.
Addressing workforce shortages isn’t only about filling today’s open roles. It’s also about thinking ahead, preparing leaders who can prevent tomorrow’s health crises and reduce strain on an overburdened system.
Going upstream with the OHSU Preventive Medicine Residency Program

CareOregon partnered with the Oregon Health & Science University (OHSU) to launch the Preventive Medicine Residency, a pioneering program that trains physicians for leadership roles in public health, policy and research. The program addresses workforce challenges by preparing doctors to think beyond individual patient care and focus on population-level health and prevention — essential for improving health outcomes.
The Program’s first cohort includes Tiantian White, MD, a family physician who grew up in rural China and saw firsthand how a lack of access to health care could have dire outcomes. “My family never had proper health care. There were so many downstream negative consequences when things became severe,” Dr. White remembers. For example, her father’s finger was injured and then amputated by someone without proper training. This led to an infection because it wasn’t properly bandaged—resulting in a hospital stay.
Experiences like this inspired White to go into preventive medicine to reduce health disparities and improve systems of care for vulnerable populations.
“These are the most mission-oriented, value-driven folks I’ve met in my career so far,” says White. “Everyone is working so hard and is passionate about what they do, despite all the looming challenges.”
While programs like OHSU’s Preventive Medicine Residency focus on preparing physician leaders with skills and knowledge to achieve long-term public health goals, many rural communities across Oregon are currently facing more urgent and severe health care workforce shortages.
Expanding rural access through Ashland Community Health Foundation
In southern Oregon, Jackson Care Connect (JCC), a coordinated care organization serving Jackson County, is part of the CareOregon family of companies. JCC partners with Ashland Community Health Foundation (ACHF) to address critical workforce gaps in the region. In this part of the state, workforce shortages can directly impact how quickly and where community members are able to receive care.
Your support plays a crucial role in enhancing my efforts to foster people in recovery.
Tom Wilson, ACHF Addiction Studies and Recovery Mentorship scholarship recipient
Stephanie Roland, ACHF’s Executive Director, says the area faces shortages at every level of the health care workforce, from medical assistants and behavioral health clinicians to specialists and emergency medical technicians (EMTs). This can lead to long wait times, even tougher to manage for the area’s significant aging population. Median wait times often exceed two weeks for primary care and can reach up to 58 days for specialists. With most services concentrated in Medford, about 15 miles away, access can be especially difficult for patients without a car or reliable public transportation.

I think [our nursing scholarship] will become even more important now that advanced nursing degrees are no longer deemed ‘professional.’
Stephanie Roland, ACHF Executive Director
To ease pressure on emergency departments and make better use of limited capacity, ACHF is supporting a new partnership with Mercy Flights that allows EMTs to respond to 911 calls even when emergency or hospital care isn’t required. Under protocols designed by Mercy Flights’ medical director, eligible patients can choose to be transported to participating urgent care clinics instead of the hospital emergency department. The model helps reduce overcrowding, shortens wait times, and ensures patients receive timely, appropriate care while preserving critical resources for life-threatening emergencies.

Investments from CareOregon and other donors have also helped ACHF expand behavioral health workforce pathways, including scholarships for future clinical mental health counselors, behavioral health internships, and continuing education for peer support specialists who plan to stay in the community. Together, these efforts help ensure that people who train in the region can continue serving their neighbors, which improves and strengthens access to care.
Even with expanded clinical and emergency capacity, many Oregonians still need support navigating complex health systems from someone in their own community who knows what they’re going through.
Building community health capacity with FolkTime
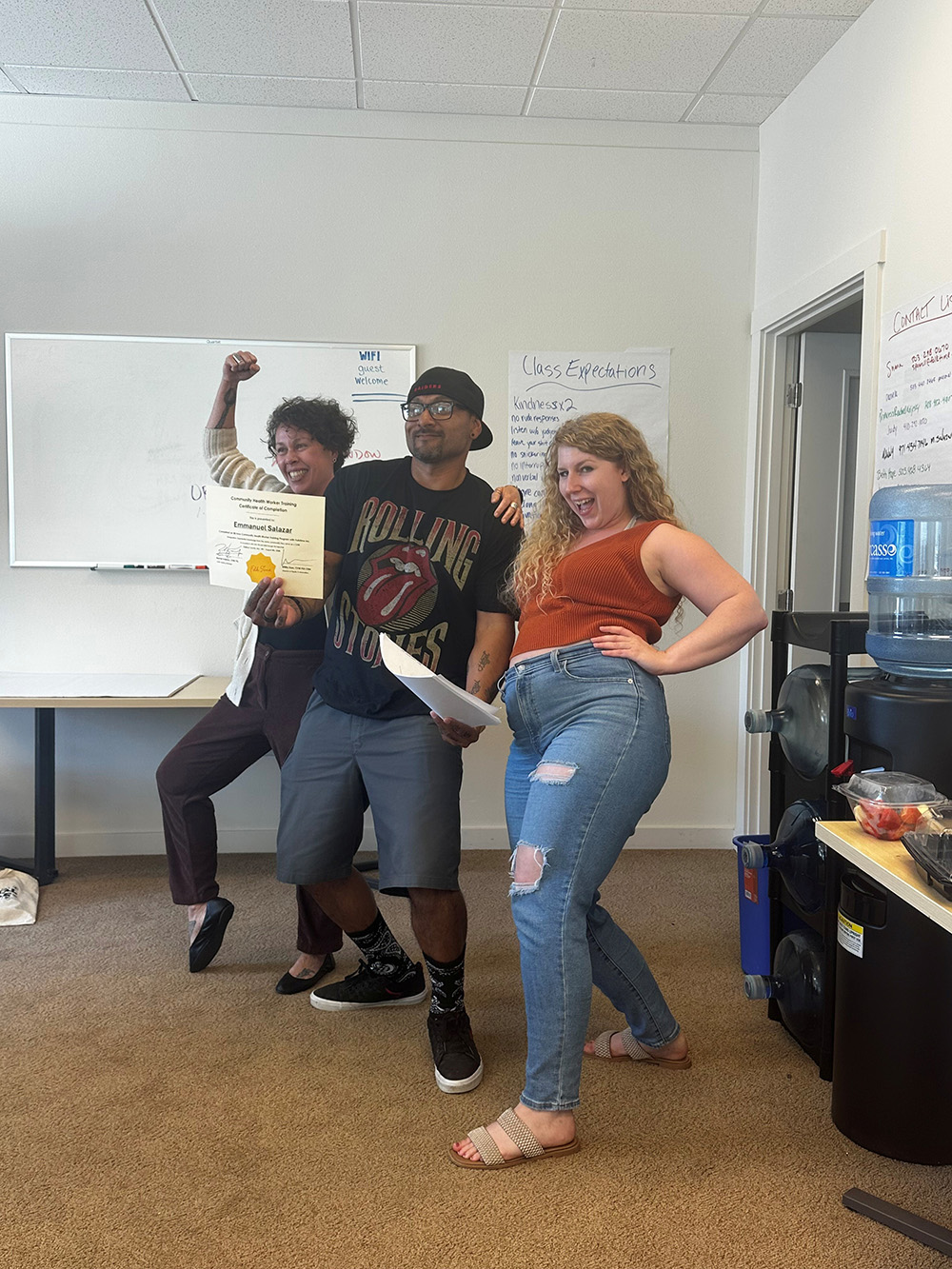
Peer support specialists, community health workers and personal health navigators play a growing role in filling workforce gaps in the health care ecosystem, and can be vital partners in addressing challenges alongside traditional models of care. FolkTime is Oregon’s oldest and longest-running peer-run organization, equipping individuals with the skills and tools to offer non-clinical support to peers for mental health and substance use disorder (SUD). CareOregon helps fund FolkTime’s peer support specialist training program, along with the state’s only personal health navigator training program providing in-person support outside of the Portland metro area, ensuring rural communities have trusted guides to help navigate complex health systems.
“Rural spaces are in desperate need of trusted people in their community to help navigate complex health systems,” notes Peter Starkey, Executive Director of FolkTme. “One of our focuses when it came to our commitment to equity was also geographic equity. A lot of people outside of the Portland-Salem area don't get access to professional development.”
For patients frustrated by provider shortages and long wait times, traditional health workers — which includes peer support specialists, community health workers and personal health navigators — can serve as a bridge and provide the support needed, right in their own community. What’s more, traditional health worker training programs are often brief, allowing graduates to begin assisting community members shortly after acquiring the necessary knowledge and skills.
“They are making people feel seen and heard, especially in a system where it can feel like you're not being heard,” Starkey adds.
The traditional health care workforce is also flexible, meaning peers can support others in a variety of settings, including within the prison system, housing services and mental health system, creating a web of support across communities. So far, FolkTime has trained over 5,000 peer support specialists in Oregon.
“Connection is what cures everything—conflict, addiction, mental health struggles,” Starkey emphasizes. “If we can connect with people more in our everyday lives, we'll be a much less lonely society.”
Why Medicaid matters in Oregon
From preventive medicine physicians to rural EMTs and peer support specialists, Medicaid helps make workforce investments like the ones highlighted here possible. By investing in innovative programs, initiatives and services like these, CareOregon is helping address today’s health challenges while training the next generation of health care workers to bring tomorrow’s solutions.
But programs like these, many of which are relatively new, depend on stable, long-term funding — primarily from Medicaid. Changes in that funding source could cause many initiatives like these to be scaled back or disappear entirely.
I don't think that philanthropy [alone] can be a solution for systems that have been eroded – it needs to be both.
Stephanie Roland, ACHF Executive Director
Investing in building and strengthening the health care workforce at every level helps ensure communities across Oregon are better equipped to meet current needs and the challenges ahead.
Investments in Action series
Our "Investments in Action" series highlights the transformative power of CareOregon's strategic investments in health and wellbeing. Through these stories, we explore how our support goes beyond traditional funding roles and is helping to close gaps in health care access and community services. Despite challenges within the Medicaid space, we remain committed to centering these important narratives of community strength and resilience.
